NABJ Black News & Views

Nadia Miller was taking a shower when she felt it. A pea-size lump in her right breast. It was 2007 and the Indianapolis, Indiana, native was just 28 years old. But at that age Miller was no stranger to breast cancer. Her older sister died of the disease when she was 30 — just two years before Miller found her lump.
“We had literally just buried my sister and we were still grieving that and then to have this disease that had already taken my sister, that was difficult all by itself to have that talk with my family because we didn’t what to expect, we just knew I was young, and I had been diagnosed with cancer and we didn’t know what was next.”
And what was next changed Miller’s life forever. She, like her sister, was diagnosed with triple negative breast cancer, an aggressive form of the disease that grows and spreads faster, has limited treatment options and worse outcomes. It’s more likely to come back after treatment than other types of breast cancer. And this cancer is more common in African American women and women under the age of 40.
What Miller discovered on her journey was that while she had “the best” doctors that she believes contributed to her survival, there were unmistakable disparities in the care Black women receive versus white women.
“I was very, very proactive in getting the information you know about my diagnosis, but the piece that was missing was the cultural differences in understanding,” she said. “There was this disconnect; we can say some of it was because of age, but some of it was because I was a Black woman and everybody that was standing around looking at me were Caucasian, 40 and older white men or Caucasian women.”
Miller’s right breast was removed and following additional testing, she learned she was BRCA positive. BRCA1 and BRCA2 are tumor suppressor genes. A positive test means there is a mutation in one of those genes and therefore a much higher risk of developing breast or ovarian cancer.
As a proactive measure, she decided to have her other breast removed as well as a total hysterectomy. She went through a year of chemotherapy and several reconstructive surgeries.
“I’ve had both my breasts removed,” she continued. “What are the side effects of chemotherapy going to look like on my skin or hair? And there weren’t books and portfolios readily available to explain it to me. And so that’s difficult. The cultural disconnect at that time, now keep in mind that was in 2007 when breast health was not being talked about the way it is now in the Black community. It just was not. And it really wasn’t being talked about publicly at the physician level either because the data hadn’t caught up with the finding, which was Black women were dying of breast cancer.”
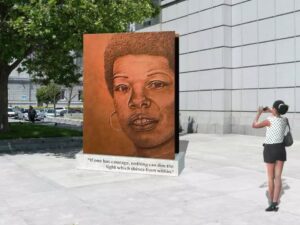
She said not seeing anybody that looks like her on brochures or pamphlets led her and her brother, John, to co-found Pink-4-Ever, Inc., to make sure minority communities, but particularly women, have access to comprehensive information, support and resources on breast cancer health and prevention.
There is no question that inequality exists. According to the National Cancer Institute, health care disparities have long been an issue in communities of color, with African Americans bearing an unequal burden of cancer compared to other groups.
Lack of insurance

Edith Mitchell, MD, is clinical professor of medicine and medical oncology at Sidney Kimmel Cancer Center at Thomas Jefferson University in Philadelphia, PA. She is also director of the center to eliminate cancer disparities and associate director of diversity affairs at Sidney Kimmel. She is one of three members on the President’s Cancer Panel.
Mitchell says lack of insurance or poor insurance is a major issue, particularly in states with no Medicaid expansion. She believes legislators need to be pushed to increase expansion so that women have greater access to good clinical care.
She says physician/clinician bias is well recognized and calls it “health care racism.”
“It means that the clinician or the healthcare system treats patients differently. And if you look at the treatment a Black person gets with the same diagnosis you will find that whites get different care than Blacks in some situations. There have also been studies conducted where the measure of the time that the patient is with the doctor is measured and guess who gets the shorter time periods? The Black patients do. So therefore, we really need to eliminate bias in health care and racism in health care systems that allow that to happen.”

Lauren Teras, PhD, Senior Scientific Director Epidemiology Research for The American Cancer Society broke it down this way:
“This is what we know: Black women are approximately 40 percent more likely to die of breast cancer than white women, despite similar incidence (new cases) rates in Black and white women. Black women are more likely to be diagnosed with breast cancer at a younger age, at a later stage (how far the cancer has spread from its original location), and to die of breast cancer even if they are diagnosed with breast cancer at the same stage as white women.”
She continued, “ Black women are also twice as likely to have an aggressive type of breast cancer (triple negative breast cancer) for which we have fewer effective treatment options. Black women are more likely to die even if they are getting mammograms as often as white women,” she said. “This Black/white mortality disparity was not always the case. In the late ‘70s and early ‘80s, breast cancer death rates were roughly the same in Black and white women. But then as major advances in early detection and treatment were made, the Black-white disparity in breast cancer mortality emerged and widened. It has held steady at 40 percent for quite some time now.”
Teras say because the underlying “why” for this disparity is complex, solutions will need to be multifaceted.
“There is a recent appreciation for these disparities in the scientific community, and it is increasingly recognized that there is a great need for more research to understand why we have such stark differences in mortality after breast cancer diagnosis by race.”
She continued, “We know that health insurance status plays a significant role, but there are likely many other factors at play. Factors hypothesized to play a role include individual and systemic racism, including unconscious implicit bias and historical residential discrimination that still plays a role today in where facilities are location, social determinants of health, including financial barriers, ability to take time off work, and childcare-related barriers…It is increasingly appreciated that not all mammograms are the same. Improving the quality of all mammograms at all facilities is of great need.”
Finding solutions
Lisa Hayes knows all about the importance of quality mammograms. In March of 2007 she felt a lump under her arm. The 64-year-old mother of three from Indianapolis, IN was unemployed and had no health insurance. She thought the lymph node was swollen because she had a cold. But over the next month it got bigger. A mammogram showed a very small tumor in her breast and the cancer had spread to the lymph node.
“When I first heard those words you have breast cancer, my mind immediately went to ‘oh well, my chances aren’t very good because I know we can’t afford treatment without health insurance,” she said.
Hayes, who was also diagnosed with triple negative breast cancer, had a lumpectomy followed by chemotherapy and radiation. She says she got good care and in what she describes as a life changing moment decided to walk away from more than 20 years as an attorney.
“I survived and for the most part had a trouble-free experience, but I also knew that that was not the case for many other women and so that led me to a job I actually started after I finished treatment with a clinic called Gennesaret Free Clinic.”
She is still Director of Women’s Health at Gennesaret where she began sharing her story, and became a living testimony, encouraging women to get mammograms.
That led to a leadership role in the community looking at what should be done to address breast cancer disparity in Black women. The RED Alliance (Reaching to End Disparities) was born with Hayes at the helm as Executive Director.
Listening
Their mission was to reduce the breast cancer mortality rate for Black women in Indianapolis. Through that work she met another breast cancer advocate—Nadia Miller.
After several years of working on the same issues, they decided to join forces and Pink-4-Ever Ending Disparities was born.
This powerful advocacy organization meets breast cancer patients where they live. In 2017 they held a series of town hall meetings on accessing breast health services. Hayes says lack of communication was a recurring theme.
“They didn’t feel like the provider was listening to them or they didn’t feel that the provider was adequately explaining things to them,” Hayes recalled. “We had numerous young women say I went to my primary care doctor, had a breast problem and that doctor said ‘oh, you’re too young to have a mammogram or you’re too young, this is not a breast-cancer-related issue and kind of blew them off despite the fact that, as we know, Black women are diagnosed at a younger age,” she said.
“So, when somebody feels like they’re not being listened to, that can have an impact. It could be that then they start to think, oh, I don’t have to worry about this, oh maybe I’m overreacting and then they choose to ignore whatever the problem, or they are turned off by that encounter with that healthcare provider but then they’re sort of put in the situation oh, I’ve got to find someone else. And sometimes it’s challenging to find someone that they feel comfortable with or someone that will take their insurance or if they’re not insured, someone who will see them without insurance.”
Worta McCaskill-Stevens, MD is an oncologist and Chief of the Community Oncology and Prevention Trials Research Group at the National Cancer Institute (NCI) at NIH. She’s involved in cancer disparities research nationally and internationally.
“It is important that African American women are informed that there are different subtypes of breast cancer,” McCaskill-Stevens said. “Most African American women get hormone responsive breast cancer despite the high visibility and frequent reporting on the more aggressive subtype of triple negative breast cancer (with biomarkers for hormones or HER2 expression). There are several advances related to triple negative breast cancer and clinical trials designed to improve outcomes among this group of patients.”
Access to clinical trials, she says, is critical in addressing these disparities in communities of color.
“As technology moves forward, it is important to encourage providers,
including primary care providers who play a major role in the management
of minority patients, African American women must participate in clinical research. Breast cancer patients also have chronic diseases that may interact with treatment or are compounded as survivors after treatment. The NCI has research trials that address treatment and cancer-related toxicities and quality of life. These trials must be promoted among the African American communities.”
Hayes and Miller are both big on clinical trials, genetic testing and knowing your family history and personal breast cancer risk but say the doctor-patient relationship is key.
“Bedside manner, that cultural competency if you will,” Miller said, “really does play a role in how we also talk to the patient. They’re not medical professionals so bringing this down into layman’s terms so a patient can understand _explaining what things mean.”
“If that provider is thinking and looking and knowing that Black woman in the context of ‘oh yes, Black women tend to be diagnosed with breast cancer at earlier ages, Black women are diagnosed with more aggressive forms of breast cancer’ that may cause that provider to treat that Black woman a little bit differently than other patients, which should be the case,” Hayes said. “That’s really what health equity is about. It’s not necessarily the same treatment, it’s treatment appropriate for that particular person that’s fair and equitable in comparison to anybody else.”