For Black Americans and the physicians who serve them, the pandemic reinforced complaints of inequities in healthcare outcomes.
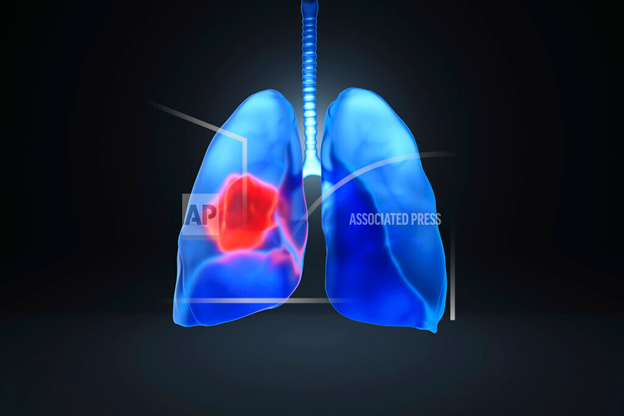
Black women have a 7% lower chance of a cancer diagnosis than white women but are 13% more likely to die. Prostate cancer death rates for Black men are more than double than those of every other racial group, according to statistics from the American Cancer Society.
Thirkield Marbury, a 72-year-old prostate cancer survivor from Ypsilanti, Michigan, began receiving regular prostate exams at 40 years old and was diagnosed in 2015.
Marbury detests “watchful waiting,” a medical practice where conditions are monitored and routine tests may be performed as opposed to medical intervention to reduce potential side-effects of treatment. It can be both effective and risky.
“That doesn’t work for Black men,” said Marbury. “Things can change very quickly in a matter of months.”
He tries to raise awareness amongst family and friends, especially other Black men, because doctors would not redress health issues unless brought to their attention by the patient, he believes.
In January 2021, the Biden administration signed an executive order to identify and study best policy practices to eliminate racial inequity within American institutions, including healthcare. The order spurred the formation of the Equitable Data Working Group, which recently completed its public comment period with the goal of enhancing data collection processes and driving policy that targets historically marginalized groups.
Still, emerging research suggests that the pandemic-driven decline in screenings could make it harder for practitioners and advocates to reduce racial disparities in cancer diagnosis and survival rates.
As healthcare providers implemented restrictions to prevent the spread of COVID-19, it meant the stop of preventative measures like cancer screenings.
A study from the Journal of the American Medical Association shows that declines in cancer screenings following the March 2020 shutdowns were sharpest in more affluent communities, those with more financial resources to access treatment to begin with. Western states had a slower screening rebound than Midwestern and Southern states, where some shutdowns were not as long or extensive.
Advancements in research, treatment programs, and access to care have narrowed the gap in cancer incidence rates among Blacks and whites.
However, death rates for Blacks are still higher than that of whites, even when cancer incidence rates between the two groups are now similar, according to the “Annual Report to the Nation on the Status of Cancer.”
For many patients, concerns about entering a healthcare environment with sick people fueled their delaying detection and prevention services.
“They were afraid of going anywhere they didn’t have to,” said Deniece Ponder, Oncology Director at the Mississippi Baptist Medical Center in Jackson, Mississippi.
The Baptist Cancer Center in Jackson, Mississippi. A month-long shutdown delayed critical early detection and prevention programs. / Google Maps capture
The Delta state has the largest Black population of any state, the highest cancer mortality rate in America, and accounts for over one-third of cancer diagnoses in the United States, according to statistics from the CDC.
The shutdown and eventual reopening meant ramping up previously underutilized services like telehealth and adopting new safety measures such as temperature checks, social distancing, and mandatory COVID-19 testing prior to one’s first visit.
Services have rebounded to pre-pandemic levels, and social media engagement spurred a 25% increase in lung screenings between April and June 2021.
But health awareness advocates indicate that long distances from treatment centers, low income, and a lack of transportation access, in addition to fear and distrust of the healthcare system, create barriers to quality, affordable treatment.
Ponder noted that some patients drive more than 50 miles from rural areas in the delta for MRIs or chemotherapy appointments. The Center’s financial assistance unit enhanced its services to provide transportation assistance and determine patient eligibility for reduced co-pays or free prescriptions.
Source: Centers for Disease Control and Prevention, Cancer Mortality by State.
In the face of renewed conversations about race in America, advocates are building upon long standing efforts that target underserved people.
The Cancer Support Community offers free, psychological support services, which help cancer patients, survivors, and their families cope with the depression, anxiety, and fatigue that also come with a cancer diagnosis.
Once a month, Marbury attends CSC of Greater Ann Arbor’s African American Fellowship, a support group specifically for Black cancer patients, survivors, and their families.
Sharing your story with others from a similar background “gives you more comfort in telling your story,” said Marbury. He also attends the prostate support group.
The AA Fellowship was the result of a lay health advisor program that trained trusted members of the community to serve as health advocates. Participants feel comfortable using CSC services because programs like the AA Fellowship make them feel “at home,” said Jamie Abelson, MSW, a member of the CSC Board of Directors.
The ACS has also intensified its efforts to address racial equity issues in health, building upon programs that reflect the Black experience, such as Partnering for Life.
As part of the program, healthcare experts built relationships with faith-based institutions in Prince George County, Maryland, issuing $6,000 grants to equip congregants with training on the importance of early detection, which was then integrated into ministry services.
Tawana Thomas-Johnson currently serves as the Vice President of Diversity, Equity, and Inclusion of ACS and is also an ordained Baptist minister.
Those doing DEI work have to know who they’re treating, said Thomas-Johnson. Early on, ACS staff determined what program participants’ experiences had been with the cancer center’s services.
“If it was favorable, that’s wonderful. But if it wasn’t favorable,” she continued, “we need to understand that if there is trauma there” to unpack it and to move through it together.”
In the immediate aftermath of former Minneapolis police officer Derek Chauvin killing George Floyd, organizations nationwide released commitment statements to diversify their workforces, pump capital into Black-owned businesses, and combat racial injustice.
While some have lived up to their promises, others have faced criticism for paying lip service to equity and inclusion.
“If you’re an organization that is committed to diversity, equity and inclusion, you’re putting resources behind it, and you’re doing work in a way that’s intentional and authentic; you ought to have outcomes,” said Thomas-Johnson.
“Within eighteen months, we saw a 47% increase in Blacks utilizing ACS programs and services,” Thomas-Johnson said of the Life initiative.
Bonnie Dockham, founding director of and current Executive Director of the CSC of Greater Ann Arbor, said it’s important to give patients and families critical information and space to make decisions about their own lives in a healthcare where many get lost due to a lack of knowledge.
For impacted-people specifically, sometimes wisdom gets the job done.
“When I got a second opinion, it made me feel better” is more receptive than “you should get a second opinion,” for example, said Dockham.
CSC membership amongst Blacks increased from 1% to 12% within 2 years after launching the AA Fellowship.
In the face of unprecedented disconnectedness brought on by restrictions on social gatherings, virtual settings are becoming a way to scale and grow community-based advocacy work.
At the University of Maryland’s Community Health and Awareness, Messages, and Prevention lab, or CHAMP, staff equip congregants with cancer awareness knowledge in an ACS-sponsored program called Project HEAL.
While Community Health Advisor trainees were already required to complete some online training in addition to the in-person sessions, CHAMP is rethinking a completely virtual format to make the program more accessible, said Nathaniel Woodard, a UMD doctoral student and graduate research assistant at CHAMP.
Woodard recognized the social and learning differences between a completely virtual and in-person setting. A previous study showed that between the two formats, trainees’ ability to educate others was similar but it took virtual learners longer to finish the material.
For Woodard, a 26-year-old Black man who grew up in the Black church and is not old enough to access certain screening services — for many of which are 40 or older — HEAL allows him to forge relationships with those who are eligible.
There is a power in someone who does not have to necessarily be concerned with these issues working toward empowering others to be aware, said Woodard.
Some CSC programs will be kept entirely remote while others are hybrid, said Abelson. The CSC purchased extra technology and designated a staff person to assist patients with operating their technology at home.
While Marbury misses the joys of being in-person, sharing his story, and hearing from others, he says that “Zoom is better than nothing.”
Moving forward, it will take renewed community engagement in the communities where it’s needed most to compel people to return to cancer centers and get screened, said Ponder.
“It really takes meeting them where they’re at.”
Amethyst J. Davis is an NABJ Media Network Casey Fellow covering health and COVID-19. She is a proud daughter of Cook County. You can follow her on Twitter @APurple_Reign.
This report was made possible with support from the Annie E. Casey Foundation.